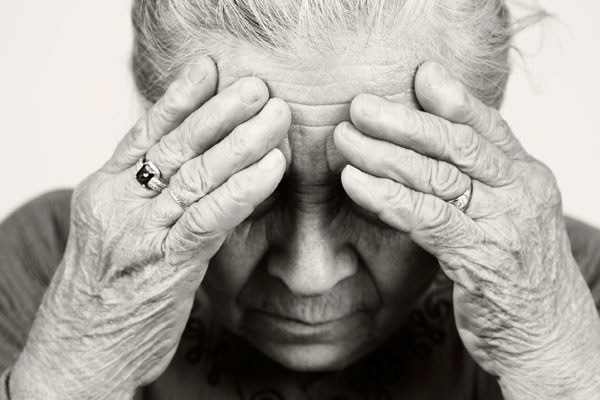
Mental health disorders affect about 20% of older adults in the U.S., according to the Centers for Disease Control and Prevention (CDC). Unfortunately, nearly one in three of those seniors doesn’t receive treatment because of shame or the fear that it will be dismissed as part of the aging process.
With knowledge and watchfulness, you can assess your senior loved one’s safety and well-being, and stay aware of their emotional and mental health to make sure they receive proper treatment.
Do mental health issues get worse with age?
Mental illness isn’t a natural part of aging. In fact, mental health disorders affect younger adults more often than the elderly, according to the National Institute of Mental Health. However, seniors are less likely to seek help.
The most common psychiatric disorder among the elderly is severe cognitive impairment or dementia. About five million adults age 65 and older — approximately 10% of seniors — have Alzheimer’s disease, according to the Alzheimer’s Association.
Depression and mood disorders affect up to 5% of seniors 65 and older, and up to 13.5% of older adults who receive home health care or are hospitalized, according to the CDC. Disturbingly, these issues often go undiagnosed and untreated.
Anxiety disorders often go along with depression. They include a range of issues, from hoarding syndrome and obsessive-compulsive disorder, to phobias and post-traumatic stress disorder. Nearly 8% of adults older than 65 have been diagnosed with an anxiety disorder at some point in their lives, says the CDC.
Risk factors for mental health disorders in seniors

Older adults experience stress like all people, but even the normal emotional and physical stresses that go along with aging can be risk factors for mental illnesses. It’s important to pay careful attention to your aging loved one’s mental health, especially if they’re living alone or aren’t able to socialize as often as they once did.
Many potential triggers exist for mental illness in the elderly, according to the World Health Organization and the Geriatric Mental Health Foundation. These include:
- Alcohol or substance abuse
- Dementia-causing illness (e.g., Alzheimer’s disease)
- Illness or loss of a loved one
- Long-term illness (e.g., cancer or heart disease)
- Chronic pain
- Medication interactions
- Physical disability or loss of mobility
- Physical illnesses that can affect emotion, memory, and thought
- Poor diet or malnutrition
Assessing mental health in older adults
One of the ongoing problems with diagnosing and treating mental illness in seniors is the fact that older adults are more likely to report physical symptoms than psychiatric complaints. In fact, many seniors may not even recognize their own mental health issues. This is why the American Psychiatric Association advises family members to seek professional advice if they believe their elderly loved one may be experiencing mental health problems.
Assess these five areas to determine whether a consultation with your loved one’s doctor is warranted:
- Life tasks and self-care activities, such as dressing, preparing meals, or using the phone
- Safety, including financial safety and driving
- Physical health, including pain or uncomfortable symptoms, hospitalizations, or loss of appetite
- Mood and brain health, such as feelings of hopelessness, loss of interest in activities they used to enjoy, or isolation
- Medication safety, including skipping medications, and worrisome side effects or symptoms related to medications
10 symptoms of mental illness in the elderly

It’s important to keep a close eye while visiting your aging loved one in order to spot signs that they need help. As your loved one ages, it’s natural for some changes to occur. Occasional forgetfulness is normal; however, persistent cognitive or memory loss can be potentially serious.
The same goes for extreme anxiety or long-term depression. Caregivers should keep an eye out for the following warning signs, which could indicate a mental health concern:
- Changes in appearance or dress, or problems maintaining the home or yard
- Confusion, disorientation, or other problems with concentration or decision-making
- Decrease or increase in appetite; changes in weight
- Depressed mood lasting longer than two weeks
- Feelings of worthlessness, inappropriate guilt, helplessness; thoughts of suicide
- Memory loss, especially recent or short-term memory problems
- Physical problems that can’t otherwise be explained: aches, constipation, etc.
- Social withdrawal, or loss of interest in things that used to be enjoyable
- Trouble handling finances or working with numbers
- Unexplained fatigue, energy loss, or sleep changes
Don’t hesitate to seek further assistance if your loved one is experiencing any of the symptoms above. Their family doctor is always a good source to start with.
…